Exodus of Doctors: A Problem That Defies Simple Solutions
Published on March 5, 2023 / Leer en español
The emigration of doctors out of Puerto Rico has raised alarms in some sectors. Many link it to the multiple problems that patients currently face with the island’s health system: lack of medical specialists in some disciplines, months-long waits for appointments, days lost in crowded medical offices, and uncertainty about the capacity of the system to adequately meet the ever-more complex health conditions of the island’s population.
According to Health Department officials, more than 8,000 doctors have ceased to practice in Puerto Rico in the past thirteen years. If we accept these numbers, the island would have lost 46% of its doctors in little more than one decade. We don’t know how much of this loss is due to emigration, or how much to deaths or retirement, but in 2017 the Department of Economic Development and Commerce (DEDC) approved the Incentives Law for the Retention and Return of Medical Professionals (Law 14) to halt, through a reduced 4% income tax rate, what it considers is an “accelerated and worrisome” migratory exodus among the island’s doctors. By 2018, 1953 medical specialists had benefited from the incentive, whose cost to the public treasury in 2021 was of $237.5 million, according to an analysis developed by Espacios Abiertos.
This fiscal incentive, however, does not seem to have been enough to curtail the shortage of doctors in Puerto Rico. According to the Financial Oversight and Management Board for Puerto Rico (FOMB), Puerto Rico currently has 72 medical areas “unattended”, with a scarcity of professionals in areas as diverse as primary medicine, mental health, or specialized medicine. It is interesting to note that the FOMB’s 2022 Fiscal Plan foresees the need for five structural reforms (human capital and social assistance, education, ease of conducting business, energy, and infrastructure), but does not include among these a comprehensive reform of the island’s health system. The Board’s recommendations focus on important albeit individual reforms to the island’s management of the federal Medicaid program, such as increasing reimbursement rates for providers and expanding eligibility levels for patients. Sixty percent (60%) of Puerto Rico’s population receive health services through Medicaid, CHIP, Medicare, and the Veteran’s Health Administration.
It is important to assess if there are other types of policies – beyond reforming the island’s administration of the federal health programs – that could or should be developed. A robust health system is necessary not only to care for an aging population, but constitutes a key pillar of any economic development strategy that involves strengthening and attracting human capital.
How to address the shortage of health professionals in Puerto Rico from a systemic or integrated point of view? In this View from Madrid I will examine some global trends about the so-called “doctor drain”; I will look into the policies implemented in Spain, from where I write this text; will contrast these measures with the situation in the USA; and will examine alternative ways to organize the health system.

The circulatory flow of doctors at a global level
According to the World Health Organization (WHO), the scarcity of health professionals is a global phenomenon, linked not only to the migration of doctors, but to demographic changes in the midst of individual societies and to technical advancements in the health-care field.
Around the world, the number of doctors and nurses who have migrated out of their country of origin has increased 60% in the past years. India, China, Pakistan, Germany, Rumania and the United Kingdom are the countries of origin from which more doctors have emigrated to work in another country. Australia, Switzerland, Israel, Ireland and Canada are the receiving countries with the highest proportion of doctors born out of the country. In the USA, where most Puerto Rico doctors migrate, almost one out of three medical practitioners is foreign-born.
The migration of professionals per se is not necessarily a negative phenomenon – it can generate, for example, flows of remittances to the home country and international networks of knowledge exchange. But in societies with fragile health systems, the exodus of professionals can indeed become problematic and cause a quasi-collapse of their health systems, with the concomitant loss of lives among the population.
Although we do not know of a formal census of doctors born or trained in Puerto Rico who are working outside the island, it is useful to examine global trends. Half of the countries that belong to the Organization for Economic Co-operation and Development (OECD), have less than 10% of its native doctors working outside the country. Spain has 3% of its native doctors working out of the country; Dominican Republic, has around 15%; Mozambique, Surinam, Barbados and Jamaica, around 45%; Samoa, 65% (see the OECD graph below). The OECD notes that Caribbean countries have been particularly affected by the emigration of its native doctors, with rates of between 50 and 75%, that is, between five and seven times the norm for half of OECD countries.
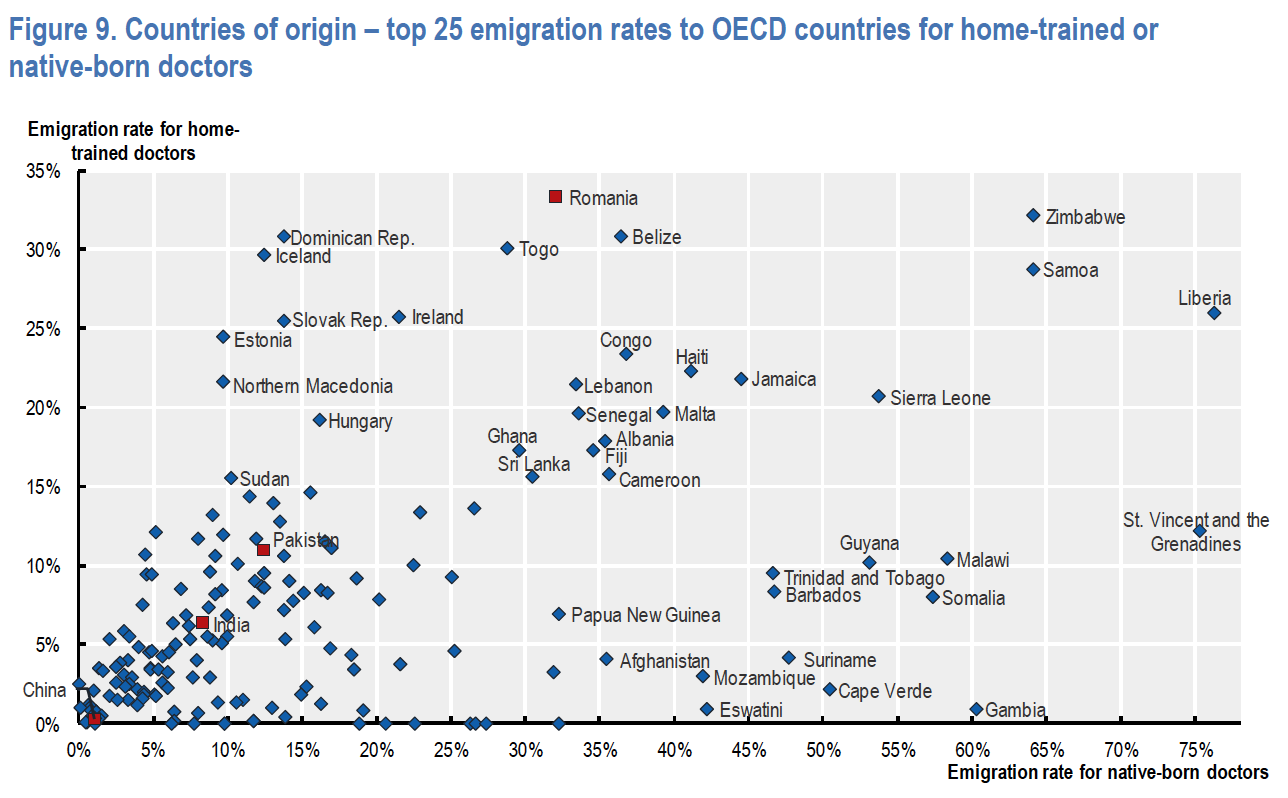
The OECD uses two parameters to evaluate the migration of doctors: those born in a country and those trained there. Source: International migration and movement of doctors to and within OECD countries, OECD Health Working Papers No. 126, p. 27.
The magnitude of this circulatory flow and its impact both in origin and receiving countries has made the mobility of health professionals a priority for entities like WHO and the OECD. These organizations have begun to look at the migratory phenomenon at a global scale. In the same vein, the European Union (EU) commissioned in 2021 – after the shock produced by the pandemic – a study on the planning systems its members have developed for their individual health labor forces – doctors, nurses and midwives. The study found that although three out of four European countries have indeed developed labor planning systems for their health structures, there are notable problems in terms of data, planning models, scarcity in certain specialties, geographical imbalances, shortages in training programs, and gaps in personnel retention systems.
In Puerto Rico, would it not be appropriate to look at the problem of scarcity of doctors and health professionals in a such a broad, systemic manner?
“Exodus of doctors”, structural imbalances and policy measures in Spain
In Spain the “exodus of doctors” has recently become a visible source of news (see for example, here and here). The Spanish health system is considered one of the best in the world, but, as has happened globally, the pandemic has left behind enormous systemic stress. In the Spanish Public Health System (“la Sanidad Pública”), 42% of patients still have access to their primary doctor the same day or the day after requesting an appointment. Wait times for specialists, however, have increased to a mean of three months, with significant differences among autonomous communities (AACC). The Basque Country registers a month-long wait; Catalonia, Aragón and Canarias, between four and five months.
It is important to note that the Spanish health system is based in the universal coverage of its population; is anchored in an extensive network of public primary facilities and hospitals; is financed by tax-revenues which the central State then distributes to the 19 autonomous communities and cities, which are the ones that then manage the system at a regional level; and coexists with an efficient and robust private insurance sector, which after the pandemic has reached 30% of penetration among the population.
In contrast to Puerto Rico, private health insurance in Spain generally works as a complement to the public health system, that is, as a system of double coverage that allows access to services not covered by the public health plan (dental or chiropractic care for example) or as a way to speed up access to specialists. Private health insurance tends to be circumscribed to civil servants, judges and military personnel, who through a system of “mutualities”, can indeed choose to substitute the public health plan for private health coverage; to the employees of large corporations who receive private health insurance as part of their benefit packages; and to the more affluent population who buys private insurance on an individual or family level.
In Spain, private health companies have their own centers for medical attention, emergency facilities and hospitals. Plans, however, are less costly than in the USA or Puerto Rico, as treatment for catastrophic or complex conditions (cancer, for example), although included in the more comprehensive private policies, tend to be referred or transferred to the public system. Likewise, most innovative last-generation treatments and cutting-edge technologies tend to be available in the private health system on a pay-for-service basis, while being available for free to participants in the public health-care system. According to the Ministry of Health, 73% of Spanish health expenditures are made by the public system (about €88,000 million or $95,000 million) versus 27% of private health expenditures (€32,000 million).
Since last year, the Spanish public health system has been shaken by strikes, protests and complaints from its doctors. These stress that the increase in patient-care quotas (up to 70 patients in one working day), the lack of investment in physical facilities and the disinvestment in primary care (which handles 80% of the health ailments of the population), has oversaturated the system. This has led to renewed public discussion about the “exodus of doctors”. The Medical College Organization claims that each year a larger number of doctors request the homologation of titles conducive to work in other EU countries. Nevertheless, the number of certificates actually requested – 4,130 in 2021 – represents only 2.1% of the 192,484 doctors that the Spanish Ministry of Health identifies as active practitioners in the country. As a matter of fact, the final migratory flow is substantially lower: between 2011 and 2020 the annual average of emigrating doctors was of 438. This would mean that the human resources shortages affecting the Spanish public health system cannot be adjudicated to the emigration of doctors, and that the phenomenon is actually one piece of a larger puzzle.
Sergi Jiménez-Martín, health economist, professor at Pompeu Fabra University and associate researcher at the Spanish think tank FEDEA, says that in the context of a common market – such as Spain and the EU or Puerto Rico and the USA – it is actually impossible to curtail the emigration of health personnel, particularly in a situation of low compensation, labor instability and poor working conditions in the country of origin. In Spain, one of the policy responses during the decade of 2000 was to facilitate the immigration of foreign-born doctors – particularly from Latin America – allowing for their direct recruitment abroad; relaxing the requirements for studying and doing their training residencies in Spain; and accrediting medicine titles obtained abroad. According to a 2015 study conducted by Universidad Complutense de Madrid, 12.5% of all registered medical practitioners in Spain were foreign-born.
Other policy measures have addressed the system’s structural human resources imbalances, always from a systemic or integral point of view. Since 2007 the Spanish Health Ministry has commissioned several studies in order to project the demographic and epidemiologic evolution of the population, quantify the future need of primary care doctors and medical specialists, and identify public policies to address the demand for health personnel. Even though the migratory flow of doctors does not seem to be large, these studies anticipate that, due to the aging process of the country’s population, by 2027 Spain will face a global deficit of 9,000 doctors. To this effect, during the past fifteen years the Council of Universities (composed by the Ministry of Education and the Council of University Chancellors) has increased the number of new university slots available for medicine studies (an increase of 44% between 2007 and 2022); has increased the number of MIR positions (the equivalent of our medical practices in the country’s hospitals); and has increased the number of doctors trained in other countries that are accepted for medical practice in Spain. The latest 2022 study emphasizes that after the shock of the pandemic, it will be necessary to implement additional measures: improve compensation packages, ensure labor stability through long-term contracts, and increase incentives for posts in rural or unattended areas.
Álvaro Hidalgo, health economist and director of the Efficiency-Based Practice of Medicine Chair for HM Hospitals, one the main private hospital networks in Spain, stresses the importance of non-economic aspects in retention schemes for doctors: the possibility of being trained in the desired specialty area (i.e., the strength and variety of medical practices), of working with cutting-edge technology, and of participating in research and clinical trials conducive to long-term experience and prestige.
What about provider rates of private plans in Spain?
In Spain, 30% of doctors work with the private health system. The rates paid by private insurers – one of the most contentious elements in Puerto Rico – are similar to those paid in the island: €18 for a patient visit to a cardiologist (about $ 19), €21 for one to a traumatologist, or €27 for a gynecologist (see the digital platform Baremos Médicos for more examples).
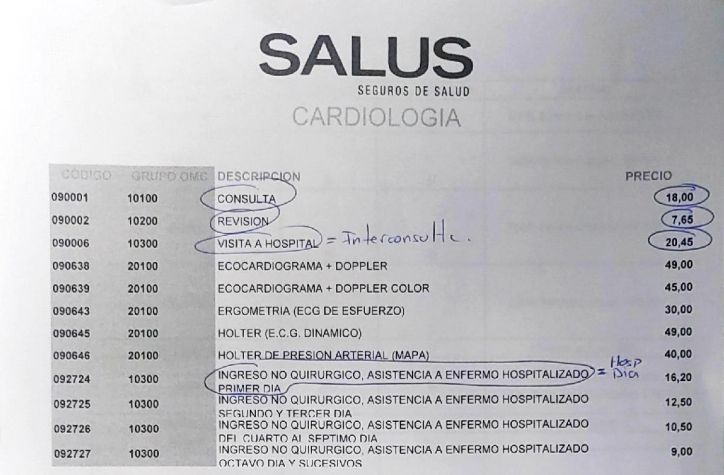
Sample of a private insurer providers’ rates chart, 2022, Spain. Source: https://baremosmedicos.com/knowledge-base/cardiologia-salus-2022
Why, then is the private health component in Spain not undergoing a crisis? Because many doctors combine posts in the public health system with contracts in private facilities: that is, the income from private insurers represents a complement to their regular income. And because the structure under which a doctor operates in Spain is substantially different from that of a doctor in Puerto Rico or the USA: many see their private patients in the insurer’s medical facilities, which means that they do not have the cost structure associated to an individually-run medical practice.
In contrast, the way medical services are organized in the USA and Puerto Rico imposes a costly structure on medical practitioners. According to a 2012 study commissioned by the Puerto Rico College of Doctors and Surgeons:
- 49% of doctors surveyed paid $100,000 annually in employee salaries
- The median rent for office space was of about $51,600 per year; mortgage payments were of about $90,000
- The median investment in purchase, repair and maintenance of medical equipment was of $135,000 per year
- Most paid between $100,000 and $300,000 per year in malpractice insurance
To all this, it would be necessary to add the $150,000 – $250,000 in student debt with which the average doctor starts its career in Puerto Rico and the USA. The cost of medicine school in the USA can oscillate between $159,000 (in a public university for residents of the state) and $256,000 (in a private university for non-residents). In Spain, in contrast, the total cost of 6 years of medicine school can range between $7,000 – $10,000 in a public university (higher ranked than private institutions) and of $54,000 – $130,000 in a private institution. Like health, education is considered one of the key anchors of the European welfare state.
The health system in the USA vs. its counterparts
Both Jiménez and Hidalgo point to the fact the USA’s health system – around which Puerto Rico’s is modeled – is a costly one. The reasons, they explain, are diverse: laissez faire in prices for both prescription drugs and medical equipment (they are regulated in Spain); the decentralization of medical and hospital providers (which duplicates administrative structures and requires providers to individually amortize costly staff and equipment); and the high remuneration received by doctors. In the USA, the average salary of a doctor is of $339,000 while in Spain it is €54,000 at the beginning of his/her career (about $58,000), €104,000 at the end. Puerto Rico falls between the two poles: according to the Puerto Rico Labor Department, the average salary for an internist in Puerto Rico is $78,700, $121,120 for those in the highest salary percentile.
These factors make the USA’s health model less cost-efficient than those of other countries. A survey prepared by the OECD in September of 2022 found that:
- The USA spends two and a half more per capita in health than its G7 counterparts: 17% of its Gross Domestic Product (GDP) versus 8.7% in the case of Italy and 11.7% in the case of Germany.
- This, however, is not translated in more health resources for the population: the USA has 2.8 hospital beds per 100,000 inhabitants versus 4.4 for the totality of OECD members. Likewise, it has 2.6 doctors per 100,000 inhabitants versus 3.6 for the OECD group.
- This larger healthcare expense is not necessarily translated into better health outcomes for the population: the USA has a higher survival rate for breast cancer patients than the OECD average (90.2% vs 84.3%), but has worse indexes in terms of effective primary care (almost double of avoidable hospital admissions for diabetes, 226 vs. 127 cases per 100,000 inhabitants, for example).
- Administrative costs for the USA’s health system are five times those of its G7 counterparts, and in general, prices for health services tend to be 27% more expensive. This makes a visit to a family doctor three times more costly in the USA than in other G7 countries.
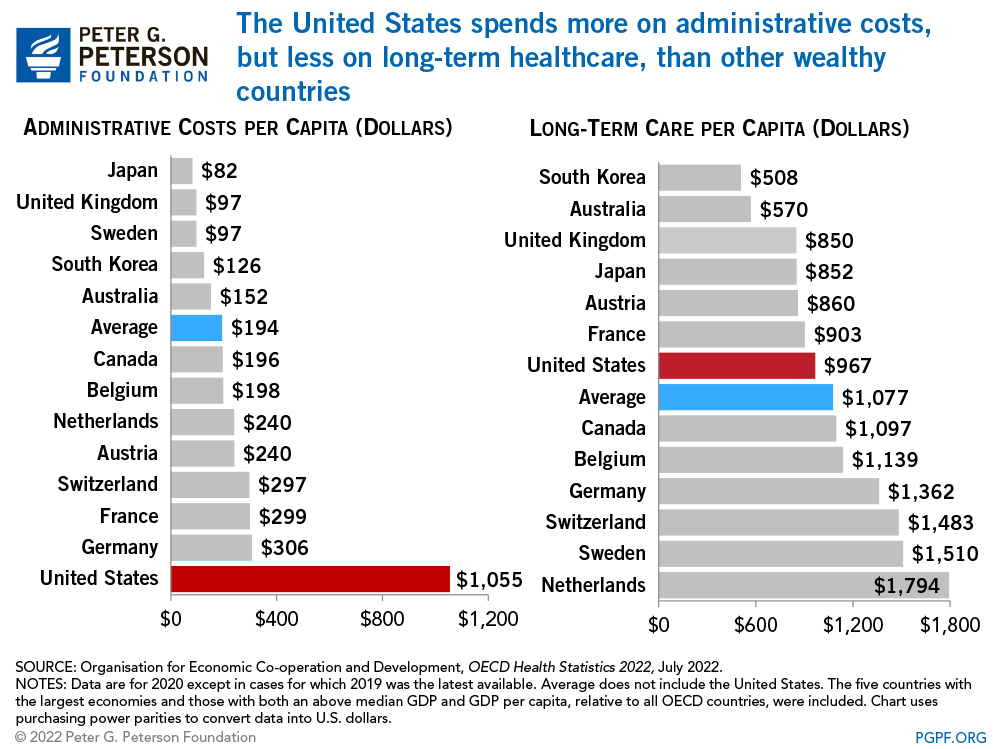
Source: Peter G Peterson Foundation, https://www.pgpf.org/blog/2022/07/how-does-the-us-healthcare-system-compare-to-other-countries
This means that health services in Puerto Rico are organized around an inherently costly health model. Jiménez thinks that, in the face of rate restrictions imposed by federal programs, an increase in tariff rates for providers serving private (individual and group) clients might not be the best idea. First, these represent only a third of the private insurance market in the island, and second, it would make insurance plans even more costly than what they are today in the island.
Rethinking the health system
Continuing to advocate for larger access to federal funding is an obvious way to address the problem, but, one may ask, should not the organization and structure of the health system itself be rethought? This is the conclusion reached by three researchers of the University of Chicago and Harvard University, who in a recently published study in January 2023 suggest that the best way to address the current failings in the USA’s health system could be the establishment of some type of universal health coverage that would allow a centralized administrative approach. Katherine Baicker, Amitabh Chandra and Mark Shepard argue that this would open the possibility of expanding the population that has access to health services (in the USA 27.5 million people, or 10.2% of the population, are currently uninsured); lower administrative costs for the totality of the system; and open the possibility of developing new provider compensation schemes based on quality and innovation (rather than on the market power of insurers and large providers). They point to the fact that, contrary to popular belief:
- Universal coverage and centralized planning systems are not necessarily based on public facilities managed by governments: there are a wide variety of practices, from Canada’s and the United Kingdom’s single payer system, to the Netherlands’ and Switzerland’s regulated markets based on private insurance and private providers.
- Universal health coverage is considered a social minimum base and coexists with private providers and insurers. France, for example, has a package of generous benefits in its universal coverage, but requires co-pays from beneficiaries; many then opt for a private health plan to cover these out-of-pocket payments (almost 90% of the population has some kind of private complementary plan). Germany, for its part, has not only supplementary private insurance plans, but allows these to actually substitute public health coverage (see for example, these two WHO compilations – here and here – for more examples).
- The system’s regulatory entity does not necessarily have to be a government agency, but may be formed by some kind of medical or private actor overseeing board.
Since the approval of the federal Affordable Care Act (ACA), better known as “Obama Care”, in 2010, several states in the USA have attempted to implement reforms to their state health systems with varied results. Twenty-one (21) states have unsuccessfully introduced state legislation to create single payer health systems and achieve universal coverage for their populations. These attempts, however, have come into conflict with federal legislation governing private health plans paid by companies and employers (ERISA). Professors Erin Brown and Elizabeth McCuskey call this jurisdictional clash a “trap of federalism” and have proposed federal law be modified: federalism, they argue, should allow states to innovate, test and learn from experimental models.
Another three states (Colorado, Nevada and Washington) have implemented more modest reforms: state health coverage anchored in the possibility offered by ACA of expanding Medicaid and establishing subsidies for private coverage. These are not universal plans and rely on the states contracting private insurers to offer the population options supervised by the government (like Plan Vital in Puerto Rico). They are sold through the state exchange markets created by ACA, from which Puerto Rico and the other territories were excluded.
Conclusion
Does Puerto Rico have some sort of judicial, political and fiscal space to reform its current health system? Could the so-called “exodus of doctors” be the spearhead to develop, in terms of public policy, a wide assessment of the island’s health system and its professionals, and evaluate how prepared the system is to address the population’s current and future health needs? Is there both will and capacity to turn Puerto Rico’s health government agencies into centers for policy innovation – like Massachusetts did in 2006 with its pioneering health reform? That is, is there the institutional will and capacity to transcend the mere administration of federal funds? The conversation is complex indeed, but with no doubt, it is worthwhile starting it.
